
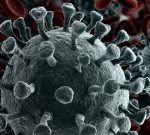
Scientists say they are seeing signs of lasting immunity to the coronavirus, even in those who only experience mild symptoms of COVID-19. A slew of studies show that disease-fighting antibodies, as well as B-cells and T-cells that can recognize the virus, appear to persist months after infections have run their course, The New York Times reported. “This is exactly what you would hope for. All the pieces are there to have a totally protective immune response,” said Marion Pepper, an immunologist at the University of Washington and an author of one of the new studies, which is now undergoing review by the journal Nature. “This is very promising,” said Smita Iyer, an immunologist at the University of California, Davis, who is studying immune responses to the coronavirus in rhesus macaques, told the Times. “This calls for some optimism about herd immunity, and potentially a vaccine.” Although researchers cannot predict how long these immune responses will last, experts consider the data to be the first proof that the body has a good chance of fending off the coronavirus if exposed to it again. “Things are really working as they’re supposed to,” Deepta Bhattacharya, an immunologist at the University of Arizona, told the Times. Bhattacharya is an author on one of the new studies, which was published on medRxiv, a pre-print server for health research that has… read on >


























-300x200.jpg)










