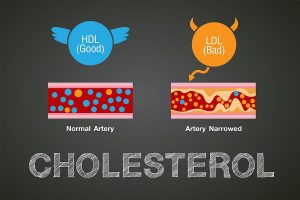
Full doses of blood thinners can benefit patients hospitalized with COVID-19, but the severity of their illness matters, researchers say. The new global analysis found that hospitalized patients with moderate COVID-19 may benefit from the drugs’ clot-preventing powers, but patients with illness so severe it requires admission to an intensive care unit may not. “SARS-CoV-2 infection can increase the risk for developing blood clots by causing a significant inflammatory response in the body,” explained Dr. Aeshita Dwivedi, a cardiologist at Lenox Hill Hospital in New York City. “These blood clots can further lead to debilitating and life-threatening conditions like heart attacks, strokes or pulmonary embolisms,” said Dwivedi, who wasn’t involved in the new study. She said the new data “has demonstrated that a higher dose of blood thinners, in addition to being safe, reduced the need for life support and possibly even death” in moderately ill patients in the hospital. Early in the COVID-19 pandemic, doctors worldwide noted that COVID-19 patients had high rates of blood clots and inflammation that led to complications, such as lung failure, heart attack and stroke. At the time, it wasn’t known whether providing COVID-19 patients with high doses of blood thinners would be safe and effective. Last December, the same group of researchers released findings showing that routine use of full-dose blood thinners in more critically ill COVID-19 patients… read on > read on >


















-300x200.jpg)